Counseling patients with diminished ovarian reserve and recurrent pregnancy loss [Study – Part II]
Let’s get on with the second part of this article:
Treatment cost increases as additional attempts are needed until the stage of embryo transfer is reached.
The cost of each failed attempt is almost 2.5 times higher compared to IVF cost. If the number of cycles needed to achieve pregnancy increases due to the very small number of blastocysts available for screening, the cost of birth becomes even greater, adding to the emotional burden of treatment.
The months of pregnancy and the moments of labor are very important to patients and particularly to women with diminished ovarian reserve.
Many argue that the time towards a successful pregnancy is shorter when IVF is performed following pre-implantation genetic screening.
However, Murugappan found that conception occurs 3.5 months earlier with management without treatment compared to IVF performed after pre-implantation genetic screening (given a strong male factor) The majority of fertile women with recurrent pregnancy loss will conceive within three months of timed intercourse, while if on IVF with pre-implantation genetic screening, they will need multiple attempts and the allocated time-frame will be exceeded in most cases.
The author of this paper defines diminished ovarian reserve as FSH > 10 IU/mL or AMH (Antimullerian Hormone) < 1.0 ng/ml.
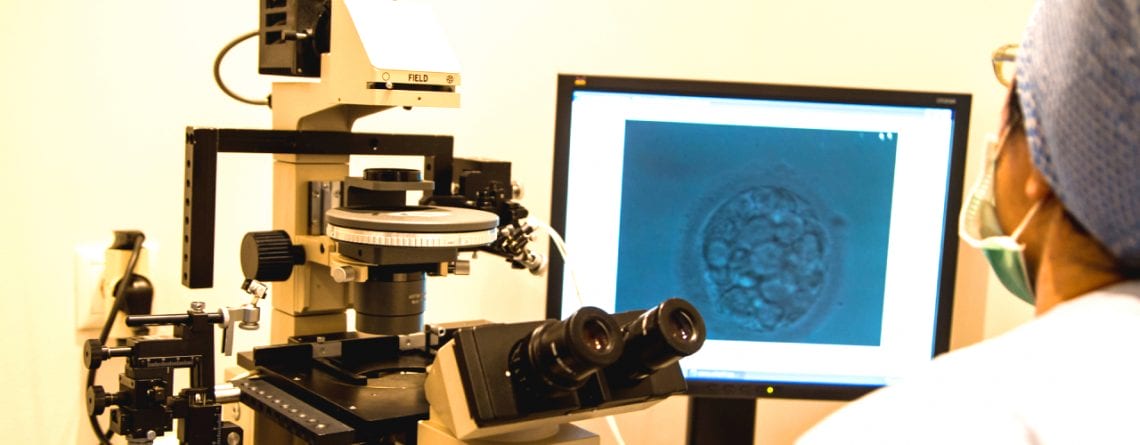
In this population, the average number of eggs retrieved was 8, and the minimum number of blastocysts submitted to screening was 3.6. Although this was lower than the respective age of women with recurrent pregnancy loss, it remains a reasonable number to proceed with IVF with preimplantation genetic screening. Some patients with severely diminished ovarian reserve will have even fewer oocytes and blastocysts. The highest maternal age in this study population was 41, and the lowest AMH was 0.4 ng/ml. Patients with severely diminished ovarian reserve had less blastocysts.
Women and physicians who support this procedure should know that the prognosis presented in this article does not apply to patients with AMH < 0.5 or women with fewer than 4 follicles, as these patients have fewer chances of having even one embryo available for transfer.
The author adds that more studies are needed to support his conclusions.
Lathi R., 2016. Caution, counseling patients with diminished ovarian reserve, and recurrent pregnancy loss about in vitro fertilization with pre-implantation genetic screening. Human Reproduction, Vol.106 , No.5, pp. 1041-1042.